Shigella and E. coli
Shigella and E. coli
The words diarrhea and dysentery have different meanings. Diarrhea, from the Greek dia, meaning “through,” and rhein, to “flow,” means watery feces, and plenty of it, often occurring frequently. Dysentery, on the other hand, is far more serious. The name also derives from the Greek, dys meaning “bad” or “abnormal,” and entera meaning bowels. We all get diarrhea occasionally, whether from an infectious disease or something we ate. Dysentery, on the other hand, is a much more serious pathological condition that makes us very ill and, in some cases, can kill us. Historically, there is good evidence that more soldiers died in some wars from the effects of dysentery than combat. Diarrhea can be troubling, sometimes a bit debilitating, but usually of limited duration. Proper rehydration is usually the only treatment needed. Dysentery, on the other hand, is a wretched illness that lays one up for days, possibly weeks. It’s usually accompanied by prostration, muscle aches, fever, and dehydration. While ill, the patient doesn’t take on proper nutrition, resulting in profound weakness. It’s a serious, unrelenting ailment.
There are quite a few microorganisms that can cause infectious diarrhea. Bacteria, viruses, and parasites all can be involved. The most serious form of diarrhea is cholera, caused by the bacterium Vibrio cholera. Cholera can be life-threatening if not treated adequately. In some people, infection with the anaerobic bacterium Clostridium difficile is of major consequence. But most infectious diarrhea is somewhat benign and lays us up for just a few days.
Dysentery usually makes us very ill. It is caused by two very different organisms, one a parasite and the other a bacterium. The parasite is an amoeba, Entamoeba histolyticum, which occurs sporadically in undeveloped countries, usually confined to a small circle of individuals. It can be a very serious infection, especially when it spreads to the liver. Diagnosis and treatment are often problematic.
The most common form of dysentery is that caused by a bacterium, a Gram-negative bacillus, so it is sometimes called bacillary dysentery. It is an ancient disease of humans; Hippocrates wrote a somewhat detailed description of it. The bacillary form of the disease can occur sporadically like the amoebic form, but it also manifests as a horrific epidemic, sickening thousands. Dysentery is especially worrisome when sanitation breaks down, such as in wars and natural disasters. When confronted as a sporadic case in a country with good medical facilities, it usually isn’t fatal unless the patient was previously debilitated with another condition. But the illness is profound, with loss of activity for days, sometimes weeks.
The organism that causes bacillary dysentery is closely related to E. coli. One could make a very good case that the organism, known to clinicians as Shigella, should more appropriately be classified in the genus Escherichia. Shigella and Escherichia are identical in 99% of their genomes. But convention and practical sharing of information demand that the name Shigella be retained. Most likely, in ancient times, members of the species E. coli began to accumulate the genes for invasive proteins, and as time went on, the distinctive creature known as Shigella came to be. Over time it became even more specialized, and today it is observed to be a distinct group.
Shigella has several characteristics that make it a unique pathogen:
It is very resistant to the effects of stomach acid and bile salts. The infective dose necessary to initiate disease is less than 100 organisms, perhaps as little as twenty. Most enteric Gram-negative rods are destroyed at a high rate by their passage through the stomach and upper small intestine, but not Shigella.
It reproduces in the small intestine. Garden variety E. coli must enter the colon to begin growing, but Shigella grows to very high numbers in the small intestine. From there, it enters the bowel in very high numbers.
As the organisms enter the colon, they encounter, to say the least, formidable competition. Even millions of them are overwhelmed by the presence of resident bowel flora that number in the billions. Shigella’s target is the lining of the bowel, especially the mast cells that serve as the entryway for several pathogens. Even though Shigella is not motile, some organisms do make it to their target site. It doesn’t attach by the end of a pilus like its E. coli relatives do, but rather by a surface protein that hooks up with a receptor on the host cell’s outer membrane. Once firmly attached, the pathogenic process begins.
Shigella’s entry into the host cell is insidious. Once bound to the host cell’s surface, the organism forms a series of proteins that create a spike that projects into the membrane of the cell it is trying to enter. It is a process like that used by Salmonella. At the end of the spike is a plug of a small protein. Once the proper interior cellular environment is detected, the plug dissolves, and several proteins enter the host cell. A couple of them induce the host cell to surround the bacterial cell with a membrane, form a vacuole, and the bacterium gains entry. After entry, the bacterium is contained in the vacuole, but the proteins that induced the penetration of the outer membrane perform a similar function to the vacuole, and the bacterium is freed inside the host cell.
Once free inside the cell, the organisms do two important things: one is to propagate, using the nutrients found in their immediate environment, and the other is to commandeer the structural proteins of the host cell, known as actin, and use them to migrate to adjoining cells. Unlike its E. coli progenitors, Shigella does not form flagella. It has the genetic material to make them, but the genes are not expressed. Rather, it takes control of actin, the host cell's proteins that are designed for structural integrity and shape, alters their direction, and rides them like a train, with the destination being the membrane of an adjacent cell.
Our cells are designed to destroy invading bacteria. By a process known as autophagy, invading microbes are encapsulated and subjected to deadly proteins. Autophagy is the “garbage disposal” of each cell, providing orderly maintenance of the by-products inevitably created during metabolism. For bacteria, being caught up in an autophagic vacuole is like being sent to jail with a death sentence. Shigella, though, produces enzymes that disrupt the system, and they can carry on their invasion.
With all this intracellular activity, the destruction of the epithelial cells lining the colon is rampant. Once engaged, the organisms stay inside the host cells, migrating from one to another, staying out of the reach of complement and neutrophils. Eventually, released cytokines like TNFa, IL-1b, and IL-8 attract large numbers of white blood cells. They also make the patient feel very ill.
With such a small number of organisms necessary to initiate an infection, it is no wonder that bacillary dysentery spreads rapidly throughout an enclosed population, especially when personal hygiene is low due to environmental factors. Shigella only grows in humans, so we don’t get it by contact with animals or eating foods associated with animal waste. It’s the classic example of “fecal-oral” transmission.
One could make a very good case that Shigella should be classified as a type of E. coli. But by convention, we recognize four distinct groups of the genus labeled as species dysenteriae, flexneri, boydii, and sonnei. These are often referred to as types A, B, C, and D instead of their species epithet. Shigella was named for Kiyoshi Shiga, the Japanese researcher who discovered and described the organism in 1898 during a severe outbreak in Japan. (Reportedly, over 20,000 people died). He named the organism Bacillus dysenterie, but in 1930 it was renamed.
In the early 20th century, as researchers worldwide studied the organism, one strain became notorious for causing an even more potent disease: Shigella dysenteriae, type 1. When epidemics were caused by this bug, bloody stools and other serious complications increased dramatically. The research discovered that these strains of Shigella had a means of virulence in addition to those of the invasive strains, namely, the formation of a toxin. Aptly, it was called Shiga toxin, abbreviated Stx.
Shigella is invasive because it contains a set of genes that code for about two dozen unique proteins. Most of these genes are not on the central bacterial chromosome but rather on a separate strand of DNA known as a plasmid. Because the proteins produced from this plasmid are necessary for invasion and virulence, it is known as the virulence plasmid or VP. Without that virulence plasmid, Shigella is just another type of E. coli.
The toxin, however, is not produced from the virulence plasmid. Instead, it comes from a very unexpected source: a virus. We often think of viruses attacking humans and other animals and plants, but viruses often infect bacteria. They are called bacteriophages, or usually just phages. Ordinarily, they are inconsequential, but rarely they take on a major role. A good example is the disease diphtheria. The organism causing diphtheria, Corynebacterium diphtheriae, is by itself innocuous. It does nothing. But C. diphtheriae infected with a particular virus becomes a virulent pathogen, producing an extremely serious disease. So it is with Shiga toxin. When Shigella is invaded by a phage known as a lambda type, it can potentially produce a toxin. And not just any toxin. Shiga toxin is the deadliest poison known to man. It has been reported that just one molecule of the stuff can kill a cell.
Several lambdoid phages can invade Shigella. The virus can insert itself into the bacteria’s chromosome, where it then lies dormant. This stage of its existence is called the lysogenic phase. Encoded on the virus is the genetic formula for the Shiga toxin, so it’s the virus that carries around the genes for the toxin, not the bacterium. As the bacterial chromosome is copied and transcribed, so are the virus and the toxin gene. Often the viral expression is suppressed, so toxin is not always produced. But, especially under stress, the Shiga toxin gene is transcribed, and the toxin flows from the organism. It is more likely to occur in times of stress, such as when the bacterium is exposed to an antibiotic.
Humans use several antibiotics that disrupt bacteria’s ability to make proteins. Drugs like tetracycline, erythromycin, and streptomycin attach to a portion of the organism’s ribosome blocking its ability to process messenger RNA. Shiga toxin acts the same way, only it acts against humans. The toxin attaches to the human 28S ribosome half of the 60S ribosome, removing a single adenine molecule. That doesn’t sound like much, but it is enough to completely halt protein synthesis in the human host cell, leading to its death. We can think of it as a “reverse antibiotic,” in which the bacteria use a drug (toxin) to disrupt human protein synthesis the same way we use antibiotics to disrupt theirs.
Shiga toxin is a complex structure. At its core is a large protein called the ‘A’ molecule. Surrounding the A portion are five ‘B’ molecules. After it is released from the bacterial cell, the toxin rolls around until one of the B molecules finds and attaches to a receptor on a human cell. The receptor has a long chemical name but is usually abbreviated Gb3. Once Gb3 on the human cell locks on to the B molecule, the whole toxin is incorporated into the host cell. Once inside, the B molecules act to free the entire molecule from the encapsulating endosome, releasing the deadly ‘A’ molecule. From there, it is just a matter of time until a portion of the A molecule hooks up with the 28S ribosome, putting the kibosh on protein manufacture and killing the cell.
Shigella and E. coli are very closely related, so it is no surprise that a virus that can infect the former can just as easily infect the latter. Several strains of E. coli are accommodative to lambda phages, but the most important for us is the one with the antigenic type of O157:h7 (it has the outer carbohydrate antigen designated 157 and the type 7 flagella). There is a slight difference in the Shiga toxins: the one on E. coli has a single amino acid difference from the one found in Shigella dysenteriae, but it acts in the same way, shutting down protein synthesis in animal cells. Since it is slightly different, the E. coli Shiga toxin is abbreviated stx1 instead of the stx found in Shigella.
E. coli O157 does not invade our cells like Shigella, moving about inside cells using actin molecules to propel itself. But it does have some characteristics which make it a formidable pathogen. Like Shigella, E. coli O157 can infect with a very small dose of organisms, most likely less than 100 bugs ingested. The organism attaches to a receptor outside of an intestinal epithelial cell. If it contains a lambda phage capable of producing Shiga toxin, serious disease may ensue.
A big difference between E. coli and Shigella is that the latter does not colonize animals other than primates. E. coli does. It is part of the normal intestinal flora of ruminants, including cows. Since such animals are an important part of our food chain, it is no surprise that an organism colonizing a cow could make its way into human food, whether it be the animal flesh itself or vegetables and fruits exposed to bovine waste matter. This situation is exasperating because adult cows are not sickened by the organism. They lack the Gb3 receptor on their cells necessary for the toxin to attach before invading. That’s not true of calves, who have an stx receptor and can get sick and perhaps die if exposed. The receptor disappears as the cow matures.
As if the E. coli variant of the Shiga toxin (stx1) wasn’t enough, a second Shiga toxin was found in E. coli, designated stx2. This second toxin is not found in Shigella, only in E. coli. It is chemically and antigenically distinct from stx and stx1, sharing only about half of the amino acid structure. But it functions the same way, with the B segments attaching and the A segment causing cellular damage. There are several subtypes of stx2, designated by subscript letters, for example, stx2a, stx2b, etc. If the culprit is of the stx2 variety, this information can come in handy in tracing the source of an outbreak.
The events in an infection caused by Shiga toxin-containing E. coli are usually straightforward. The patient eats some food contaminated with the organism. Like Shigella, the number of organisms required to set up an infection is extremely low, probably less than a hundred bugs. Organisms then attach to the cells lining the colon by a bacterial surface protein known as intimin. E. coli O157 is rich in this substance. Sometimes the organism just sits there, not doing much. After all, the virus within it bears the genetic code for the toxin, and the virus’ genes are sometimes suppressed. But once activated, toxins pour forth from the bacteria, attaching themselves to the intestinal epithelium and entering the bloodstream. The illness thus shows considerable variability in infected patients: the higher the dose of infecting bacteria, the more accommodative the patient’s bowel is to the bacteria’s multiplication, and the more active the virus within the bacteria, the higher the toxin release and the more severe the illness.
The toxin acts on two fronts. In the intestine, it attaches to the bowel lining, leading to its erosion and hemorrhagic diarrhea. The toxin also enters the bloodstream, and as it circulates through the body, it randomly attaches to the Gb3 receptors of the cells lining blood vessels, the endothelium. It concentrates most in the kidneys, where some cells have a high level of Gb3. It is most aggressive in the cortex of the kidney, in the renal tubules. As these cells are poisoned by the toxin and slough off, collagen exposure results. This activates platelets, which leads to the activation of thrombin and the laying down of clots. If enough renal tubules are damaged, kidney damage is profound, leading to incomplete filtering of the blood and the build-up of the waste product urea in the bloodstream, a condition known as uremia.
The toxin causes similar damage to other parts of the body with the attendant build-up of platelets and mini clots. As red blood cells flow through the blood vessel, they can bump into these irregular surfaces and become damaged. The damaged red blood cell is known as a schistocyte (from the Greek, schistos, or divided). Such cells are highly susceptible to breaking apart and releasing their hemoglobin, which damages the kidneys when free.
This cascade of events is known as the “hemolytic-uremic syndrome,” or HUS. It can be deadly. When medical intervention is available, including fluid replacement and dialysis, the patient usually survives, but sometimes severe kidney damage results. As in most cases, when the afflicted patient is very young or very old or encumbered by a pre-existing medical condition, the outcome becomes potentially more critical.
Tracing the source of a toxigenic E. coli outbreak can be difficult, if not impossible. If it occurs in a restaurant, and meat is the common source of infection, it is usually not too hard to discover the source of the offending food. But if the organism is contaminating fresh produce, like lettuce, it becomes very challenging to find where it came from and if it can occur again. The cows responsible are not sick. Investigators can’t simply go to local veterinarians and ask them how many sick cows they’ve treated. Epidemiologists and lab workers require intense work to discover the strain of the organism involved and its common source.
Shigella and E. coli are bacteria; in the lab, it is very easy to kill them with an appropriate antibiotic. Unfortunately, for diseases in humans, it doesn’t work that way. Shigella is an intracellular pathogen, so the antibiotic must penetrate tissues to reach the organism. Experience has shown that antibiotic treatment, even when the bug is highly susceptible to the drug, does not hasten the course of the disease. With toxigenic E. coli, using an antibiotic stresses the virus responsible for toxin production, inducing it to produce more of it, ironically worsening the situation. Palliative treatment is all that can usually be done.
Shiga toxin is known as an exotoxin. It is made inside the bacterial cell, then released to do its damage in areas remote from the bug that made it. It differs from endotoxin, the lipid A component of Gram-negative bacteria cell walls that all strains of E. coli possess. Endotoxin does not come into play for stx-positive strains. While sitting in the bowel cranking out the toxin, they are no different from any other strain of E. coli. The exotoxin does its dirty work remotely from the organism that produced it.
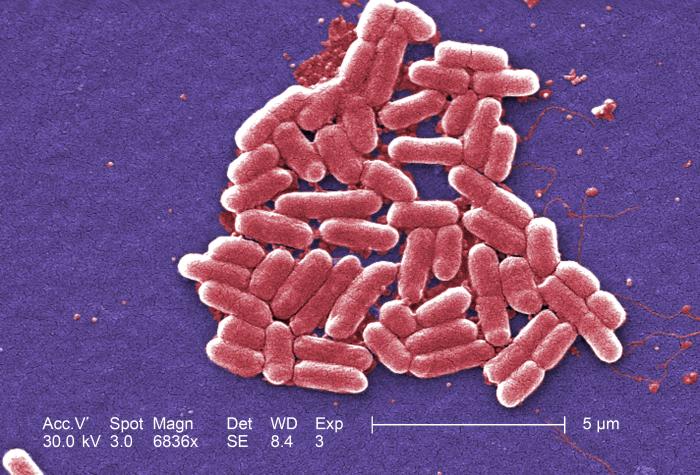
Micro colony of Enterohemorrhagic Escherichia coli, O157 (PHIL)